Testosterone is much more than just the male sex hormone - it is a fundamental building block in the body's hormonal balance, affecting everything from muscle mass and bone strength to sex drive and mental well-being. Although primarily associated with men, testosterone also plays an important role in women, and understanding this complex hormone is essential for optimal health throughout life.
In this comprehensive guide, we will explore the many facets of testosterone: from its basic function in the body to the causes of low testosterone levels, the symptoms to look out for, and the treatment options available. We will also delve into natural ways to optimize your hormone levels and address the risks associated with testosterone abuse.
What is testosterone?
Testosterone is the primary male sex hormone, produced mainly in the testicles of men. This androgenic steroid hormone is responsible for the development and maintenance of male secondary sex characteristics, including increased muscle mass, a deepening voice, and facial and body hair.
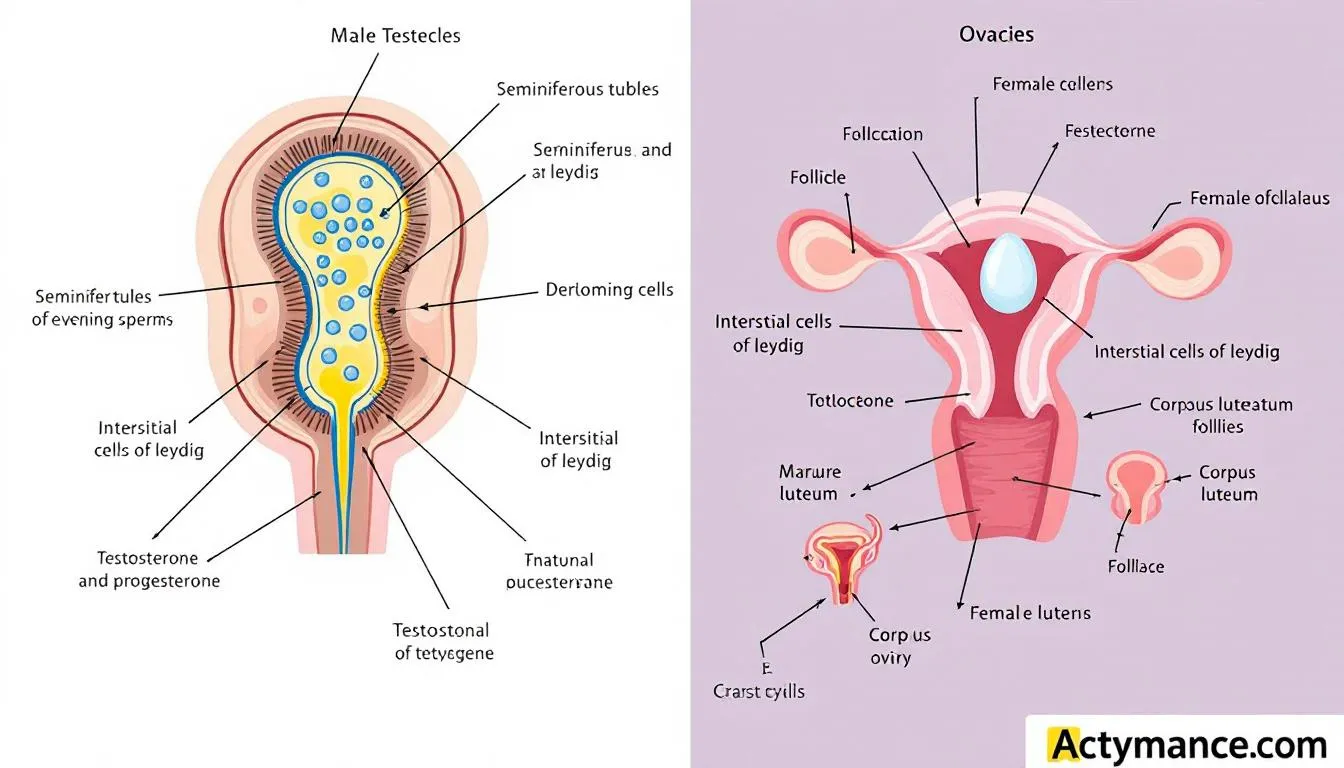
In women, testosterone is produced in smaller amounts in the ovaries and adrenal glands. Although women have significantly lower testosterone levels than men, the hormone is still essential for their ovarian function, bone strength, and potentially libido.
Testosterone acts as an anabolic hormone, meaning it promotes tissue growth and repair. It affects:
- Muscle growth and strength
- Bone strength and density
- Body fat distribution
- Red blood cell production
- Sperm production in men
An important distinction to understand is the difference between total testosterone and free testosterone. Most testosterone in the blood is bound to proteins, primarily sex hormone binding globulin (SHBG) and albumin. Free testosterone is the part of the hormone that is not bound to proteins and is therefore biologically active and available to the body's cells.
How does testosterone work in the body?
Testosterone's effects on the body begin during fetal life, where it controls the formation of male sex organs from as early as 7 weeks of gestation. During puberty in boys, typically between the ages of 9-14, testosterone drives dramatic physical changes.
- Puberty-related changes include:
- Genital growth and maturation
- Voice changes and deepening of the voice
- Increased height and muscle mass
- Initiation of sperm production
- Development of facial and body hair
In adult men, testosterone maintains a number of vital bodily functions. The hormone affects muscle mass by increasing protein synthesis and reducing protein breakdown. This results in increased muscle strength and volume, especially when combined with resistance training.
Testosterone also affects fat distribution in the body. Low testosterone levels are often associated with increased belly fat and decreased muscle mass, while normal levels help maintain a healthier body composition.

The hormone's influence on sex drive and sexual function is well documented. Testosterone influences libido through its effects on the brain and neural circuits that control sexual behavior. Reduced testosterone levels can lead to decreased libido and sexual problems.
A fascinating aspect of testosterone's function is its conversion into other hormones. Through the enzyme aromatase, testosterone can be converted into estradiol, a form of estrogen that is vital for both male and female reproductive functions. Testosterone can also be converted into dihydrotestosterone (DHT), which is more potent at the androgen receptor and is primarily responsible for prostate growth and hair patterning.
Normal testosterone levels and age-related changes
Understanding normal testosterone levels is essential for assessing hormonal health. Testosterone levels vary significantly between individuals and are affected by factors such as age, time of day, and general health.
Reference values for testosterone
|
Sex |
Normal testosterone level |
|---|---|
|
Adult men |
300-1000 ng/dL (10.4-34.7 nmol/L) |
|
Adult women |
15-70 ng/dL (0.5-2.4 nmol/L) |
It is important to note that testosterone levels vary throughout the day, with the highest values typically in the morning and the lowest in the evening. This diurnal variation is a normal part of the body's hormonal rhythm.
Starting around the age of 30, men begin to experience a gradual decline in testosterone production. This age-related decline is typically around 1-2% per year, meaning that a 60-year-old man may have 30-40% lower testosterone levels than in his youth.
Factors that influence age-related changes:
- Natural aging: The Leydig cells in the testicles become less efficient at producing testosterone
- Increased SHBG: Sex hormone-binding globulin increases with age, reducing the amount of free testosterone
- Lifestyle factors: Obesity, lack of exercise, and poor sleep accelerate the natural decline
- Medical conditions: Diabetes, cardiovascular disease, and other chronic conditions can affect testosterone production
The difference between total testosterone and free testosterone becomes especially relevant with age. While total testosterone levels may only decrease moderately, the increase in SHBG may mean that free testosterone decreases more significantly, which can result in symptoms of testosterone deficiency even with normal total testosterone levels.
Causes of low testosterone
Low testosterone levels, also known as hypogonadism, can have many different causes. Understanding these causes is essential for proper diagnosis and treatment.
Primary Testosterone Deficiency (Hypergonadotropin Hypogonadism)
Primary testosterone deficiency occurs when the problem lies in the testicles themselves. In this case, the pituitary gland will try to compensate by producing more luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Causes of primary testosterone deficiency:
- Klinefelter syndrome: A genetic condition in which men have an extra X chromosome
- Injury to the testicles: Trauma, infection, or surgery
- Chemotherapy and radiation therapy: Can permanently damage the testicles
- Autoimmune conditions: The body's immune system attacks the testicles
- Aging: Natural decline in testicular function
Secondary testosterone deficiency (hypogonadotrophic hypogonadism)
Secondary testosterone deficiency occurs when the problem lies in the pituitary gland or hypothalamus, which is not sending the right signals to the testicles. In this case, both LH, FSH, and testosterone will be low.
Causes include:
- Pituitary tumors: Can affect hormone production
- Medications: Certain medications can suppress hormone production
- Chronic diseases: Liver disease, kidney disease, and other systemic conditions
- Past use of anabolic steroids: Can suppress the body's natural hormone production
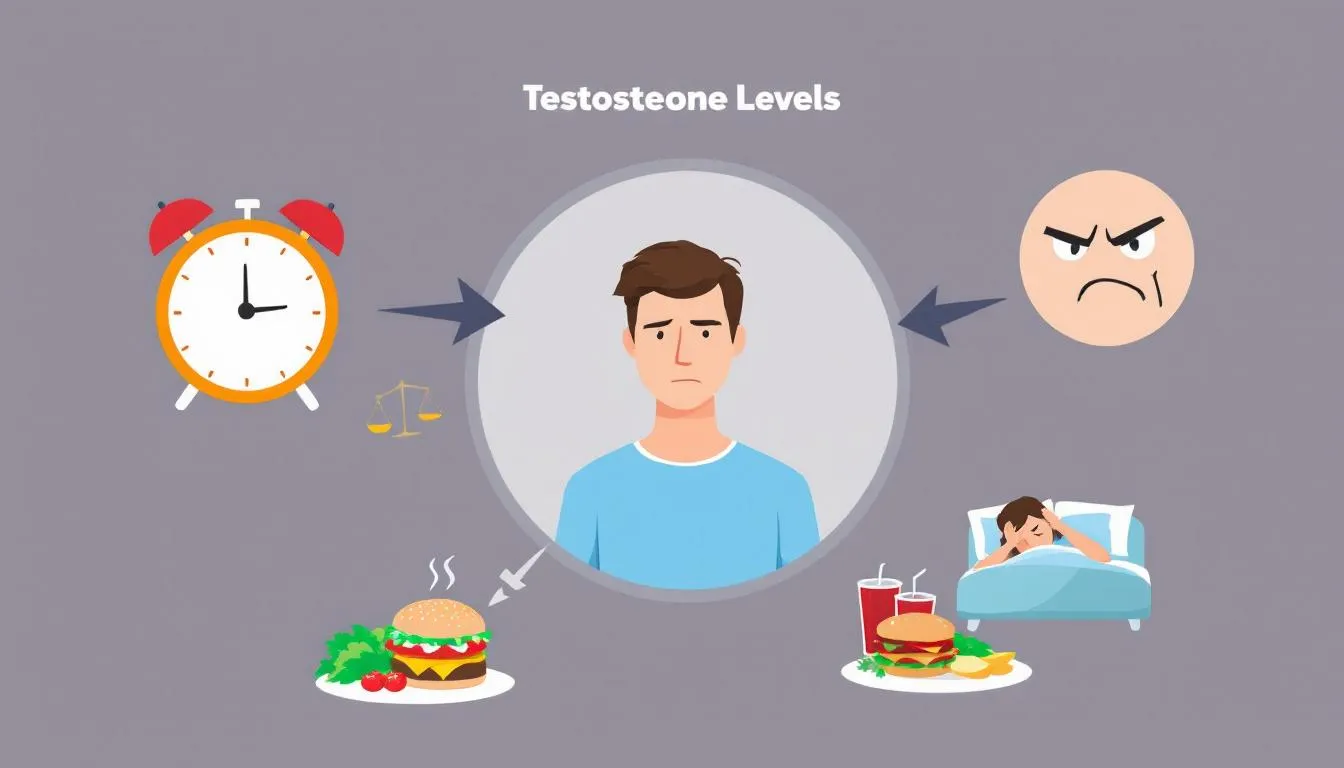
Lifestyle factors that affect testosterone
Many lifestyle factors can have a significant impact on testosterone production, and these are often modifiable through behavioral changes.
Obesity and Testosterone
Obesity has a particularly negative impact on testosterone levels through several mechanisms:
Increased aromatase activity: Adipose tissue contains the enzyme aromatase, which converts testosterone to estrogen
Inflammation: Chronic inflammation from obesity can affect hormone production
Insulin resistance: Can affect the hypothalamic-pituitary-gonadal axis
Reduced SHBG: Leads to increased clearance of testosterone from the blood
Sleep deprivation and hormone production
Sleep is crucial for hormone production, as most testosterone is produced during REM sleep. Studies show that men who sleep less than 5 hours per night can have up to 15% lower testosterone levels than those who get 8 hours of sleep.
Chronic Stress and Cortisol
Continued stress leads to elevated cortisol, which directly inhibits testosterone production. Stress also affects the hypothalamic-pituitary-gonadal axis and can result in decreased libido and sexual dysfunction.
Alcohol and the Testicles
Excessive alcohol consumption has a direct toxic effect on the testicles and can also affect the pituitary gland. Chronic alcohol abuse is associated with significantly reduced testosterone levels and can lead to permanent damage to hormone production.
Symptoms of low testosterone
The symptoms of low testosterone can be subtle and develop gradually over time, making it difficult to recognize the condition. Symptoms also vary significantly between individuals and are influenced by factors such as age, general health, and the degree of testosterone deficiency.
Physical Symptoms
- The physical symptoms of low testosterone include:
- Reduced muscle mass and strength
- Gradual loss of muscle mass, especially in the arms and legs
- Reduced muscle strength and endurance
- Increased difficulty building muscle through exercise
- Increased fat storage, especially around the stomach
Bone problems
- Reduced bone mass and increased risk of osteoporosis
- Increased risk of bone fractures
- Joint pain and stiffness
Energy and fatigue
- Increased fatigue and exhaustion, even after adequate rest
- Reduced energy and motivation for daily activities
- Needing more sleep than usual
Other physical symptoms
- Weight gain, especially belly fat
- Reduced body hair and slower beard growth
- Blemished skin or changes in skin texture
- Sensitivity to cold

Sexual Symptoms
Testosterone's role in sexual function means that low levels often result in:
Reduced libido and sex drive
- Significantly reduced interest in sexual activity
- Fewer spontaneous erections, especially in the morning
- Reduced sexual fantasy and thoughts
Erectile dysfunction
- Difficulty achieving or maintaining erections
- Reduced quality of erections
- Problems with sexual performance
Reduced sperm quality
- Reduced semen volume
- Reduced sperm motility and concentration
- Potential fertility challenges
Mental symptoms
The psychological aspects of low testosterone levels are often underestimated, but can have a significant impact on quality of life:
Depression and mood swings
-
Feelings of low spirits or depression
-
Irritability and mood swings
-
Increased emotional reactivity
Cognitive impact
-
Difficulty concentrating and decreased focus
-
Memory problems
-
Reduced motivation and drive
-
Feeling of “mental fog”
Self-esteem and self-confidence
-
Decreased self-confidence, especially in relation to masculinity
-
Feeling of having lost energy and vitality
-
Social withdrawal
Differences between younger and older men
The symptoms of low testosterone levels can manifest differently depending on age:
Younger men (under 40)
- Often more pronounced sexual symptoms
- Rapider loss of muscle mass
- More pronounced impact on energy and motivation
Older men (over 50)
- Symptoms can be confused with normal aging
- More subtle changes over time
- Increased focus on bone health and cardiovascular risk
Diagnosing testosterone deficiency
Proper diagnosis of testosterone deficiency requires a careful combination of clinical assessment and laboratory results. Diagnosis can be complex due to the nonspecific nature of symptoms and the natural variations in testosterone levels.
Clinical assessment
The first part of the diagnosis involves a thorough history and physical examination. The doctor will focus on:
Symptom assessment
- Detailed review of physical, sexual, and psychological symptoms
- Time of onset and progression of symptoms
- Impact on daily activities and quality of life
Medical history
- Previous illnesses and surgeries, especially related to the testicles or pituitary gland
- Current medications, including opioids, steroids, and antidepressants
- Family history of hormonal conditions
Lifestyle factors
- Sleep patterns and quality
- Alcohol and substance abuse
- Exercise and dietary habits
- Stress levels and mental health
Blood tests and laboratory values
The laboratory diagnosis of testosterone deficiency is based on several hormones and biomarkers:
Primary measurements
- Total Testosterone: Ideally measured in the morning (between 7-11am) due to circadian variation
- Free Testosterone: Calculated or measured directly to assess biologically active hormone
- SHBG: Sex Hormone Binding Globulin affects the amount of free testosterone
Secondary Hormone Measurements
- LH (Luteinizing Hormone): Helps differentiate between primary and secondary hypogonadism
- FSH (Follicle Stimulating Hormone): Assesses pituitary function
- Prolactin: Elevated levels can suppress testosterone production
Timing and Repeated Measurements
Due to the natural variability in testosterone levels, proper timing and repeated measurements are essential:
Optimal timing
- Blood samples should be taken in the morning (7-11) when testosterone levels are highest
- Avoid sampling during acute illness or stress
- The patient should be fasting and have slept normally the night before
Confirmation of the diagnosis
- At least two separate measurements with low testosterone levels
- Measurements taken 2-4 weeks apart
- Consistent symptoms that correlate with low laboratory values
Further tests
In some cases, further tests may be needed:
Imaging
- MRI scan of the pituitary gland if a tumor is suspected
- Ultrasound of the testicles if there are physical abnormalities
Specialized tests
- GnRH stimulation test to assess pituitary response
- Bone densitometry if osteoporosis is suspected
Treatment of testosterone deficiency
Treatment of testosterone deficiency requires careful consideration of the patient's symptoms, laboratory values, age, and general health. The goal of testosterone therapy is to restore normal physiological levels and alleviate symptoms while minimizing risks.
Indications for testosterone therapy
Treatment is indicated when there is:
- Confirmed low testosterone levels through repeated measurements
- Symptoms consistent with testosterone deficiency
- Absence of contraindications
- Patient's desire for treatment after thorough information
Different forms of treatment
There are several methods of testosterone replacement, each with its own advantages and disadvantages:
Gels and creams
- Daily application to the skin, typically on the shoulders, upper arms or abdomen
- Advantages: Physiological absorption, easy to adjust the dose
- Disadvantages: Risk of transmission to other people, skin reactions
- Requires caution when coming into contact with partners and children
Transdermal patches
- Applied daily to the skin, often on the back or thigh
- Advantages: Constant release throughout the day
- Disadvantages: Frequent skin reactions, visible patches
Injections
- Intramuscular injections every 2-4 weeks or longer intervals with depot preparations
- Advantages: Good compliance, controlled dosage
- Disadvantages: Fluctuations in testosterone levels, discomfort during injection
Subcutaneous pellets
- Small testosterone pellets implanted under the skin every 3-6 months
- Advantages: Long-lasting effect, good patientcompliance
- Disadvantages: Less flexibility in dosing, surgical procedure
Dosage and Adjustment
Initial dosage and subsequent adjustments are based on:
- Patient's baseline testosterone level
- Severity of symptoms
- Response to treatment
- Adverse effects and tolerability
The goal is to achieve testosterone levels in the lower-middle range of normal for young adult men (400-700 ng/dL). Treatment is adjusted individually based on symptom improvement and laboratory follow-up.
Medical follow-up during treatment
Regular monitoring is essential for safe and effective treatment:
Initial follow-up (3-6 months)
- Assessment of symptom improvement
- Testosterone level and dose optimization
- Screening for early side effects
- Hematocrit (risk of polycythemia)
Annual follow-up for stable treatment
- Complete blood count (hematocrit, hemoglobin)
- Liver and kidney function
- Lipid profile and cardiovascular risk factors
- PSA and prostate assessment in men over 40 years
Specific monitoring parameters
- Hematocrit: Should be kept below 54% to avoid increased risk of thrombosis
- PSA: Annual measurement in men over 40 years
- Bone density: Baseline and follow-up for osteoporosis
- Sleep apnea: Screening if symptoms are present
Side effects and contraindications
As with any hormonal treatment, testosterone replacement can have side effects and is not suitable for all patients. Understanding the risks is essential for making informed treatment decisions.
Common side effects
Mild to moderate side effects
- Acne and oily skin, especially at the beginning of treatment
- Fluid retention and slight weight gain
- Increased body hair
- Mood swings and irritability
- Sleep disturbances
- Skin-related side effects
- Skin reactions to gels and patches
- Increased sweating
- Blemished skin, especially in people with a history of acne
Serious side effects
- Polycythemia and blood-related risks
- Increased red blood cell production can lead to polycythemia
- Increased risk of blood clots and thromboembolic events
- Requires regular monitoring of hematocrit
Cardiovascular risks
- Controversial evidence regarding cardiovascular disease
- Possible increased risk of heart attack and stroke in older men
- Impact on cholesterol profile and blood pressure
Prostate disease
- May accelerate the growth of existing prostate cancer
- Increased risk of benign prostatic hyperplasia
- Regular PSA monitoring is essential
Sleep apnea
- Testosterone may worsen existing sleep apnea
- Increased risk of developing sleep apnea in predisposed individuals
- Contraindications
Testosterone therapy is not suitable for:
Absolute contraindications
- Active or suspected prostate cancer
- Active breast cancer in men
- Untreated severe sleep apnea
- Untreated severe heart failure
Relative contraindications
- Previous prostate cancer (requires specialist assessment)
- Severe cardiovascular disease
- High hematocrit or polycythemia
- Severe liver or kidney disease
Special considerations for fertility treatment
Testosterone treatment may affect sperm production and fertility:
- Exogenous testosterone suppresses pituitary release of LH and FSH
- This can lead to decreased sperm production and testicular atrophy
- The effect is often reversible, but may last for months after cessation
Alternative treatments such as hCG or clomiphene may be considered in men with fertility treatment
Natural ways to increase testosterone
Although medical treatment may be necessary for severe testosterone deficiency, many men can benefit from natural approaches to optimizing their hormone levels. These lifestyle changes can be especially effective for mild to moderate testosterone deficiency.
Lifestyle changes for hormone optimization
Weight Loss and Body Composition
- Losing excess body fat, especially belly fat, can significantly improve testosterone levels
- Aim for a body fat percentage of 10-15% for men
- Gradual weight loss (0.5-1 kg per week) is most sustainable
- Combine calorie reduction with resistance training to preserve muscle mass
Regular exercise and training
- Resistance training and weight training have the strongest effect on testosterone
- Compound exercises such as squats, deadlifts and bench presses are particularly effective
- High-intensity interval training (HIIT) can also increase testosterone levels
- Avoid overtraining, as this can have the opposite effect
Stress management and mental health
- Chronic stress and elevated cortisol suppress testosterone production
- Effective stress management techniques include meditation, yoga and deep breathing
- Regular relaxation and hobbies can reduce stress levels
- Professional help for severe stress or depression
Sleep optimization
Sleep is crucial for hormone production and should be a high priority:
Sleep hygiene principles
- 7-9 hours of quality sleep per night
- A consistent bedtime and wake-up time, even on weekends
- A dark, cool, and noise-free bedroom
- Avoid screens and stimulating activities 1-2 hours before bedtime
Factors that improve sleep quality
- Regular exercise (but not late in the day)
- Healthy diet and avoiding large meals before bedtime
- Limited caffeine after 2 p.m.
- Exposure to natural light in the morning
Dietary optimization for hormone production
A healthy diet plays a key role in hormone production and can significantly affect testosterone levels:
Macronutrients
- Adequate protein: 1.6-2.2 g per kg of body weight to support muscle mass
- Healthy fats: 20-35% of total calories, focus on omega-3 and saturated fats
- Complex carbohydrates: To support energy production and hormone balance
Important foods for testosterone production
- Lean protein sources: Meat, fish, eggs and legumes
- Healthy fats: Nuts, avocado, olive oil and fatty fish
- Zinc-rich foods: Oysters, meat, nuts and seeds
- Vegetables: Especially leafy greens and cruciferous vegetables
Foods and substances to avoid
- Excessive alcohol intake
- Processed foods and trans fats
- High sugar intake and refined carbohydrates
- Soy in large quantities (controversial)
Effective supplements for testosterone
Although a healthy diet is the foundation, certain supplements can be beneficial in case of deficiency conditions:
Tongkat Ali
- Natural herb that can support the body's own testosterone production
- May contribute to increased energy, muscle mass and libido
- Dosage: 200–400 mg daily (standardized extract of 2%–3% eurycomanone)
- Should be taken in cycles, e.g. 8 weeks on, 2 weeks off
Tongkat Ali can be purchased here: Uniiq Tongkat Ali
Zinc
- Essential mineral for testosterone production
- Especially effective for zinc deficiency
- Dosage: 8-11 mg daily, do not exceed 40 mg
- Best absorbed on an empty stomach
Vitamin D
- Supports hormone production and immune function
- Especially important during the winter months in Denmark
- Dosage: 10-20 micrograms daily, more if deficiency is detected
- Fat-soluble vitamin, must be taken with food
Magnesium
- Important for energy production and hormone balance
- Supports sleep quality and stress management
- Dosage: 350-400 mg daily
- Can cause stomach upset in high doses
Omega-3 fatty acids
- Anti-inflammatory properties
- Supports cardiovascular health and hormone production
- Dosage: 1-3 g EPA+DHA daily
- Choose quality preparations tested for heavy metals
Adaptogenic herbs
- Ashwagandha: May reduce stress and increase testosterone
- Rhodiola: Helps with stress management and energy
- Dosage and quality vary, choose standardized extracts
Anabolic steroids and testosterone as doping
It is important to distinguish between medical testosterone therapy and illegal use of anabolic steroids. While testosterone replacement under medical supervision aims to restore normal physiological levels, steroid abuse often involves high doses of synthetic androgens with serious health risks.
Difference between medication and abuse
Medical testosterone therapy
- Dosing aims for normal physiological levels
- Regular medical monitoring and follow-up
- Treats documented hormone deficiency
- Focus on symptom relief and quality of life
Steroid abuse and doping
- High doses, often 10-100 times medical doses
- No medical monitoring
- Goals of increased muscle mass and performance
- Often combined with other anabolic steroids (“stacking”)
Health risks of overdose
Misbrug af anabole steroider kan føre til alvorlige og potentielt livstruende komplikationer:
Cardiovascular complications
- Increased risk of heart attack and stroke
- High blood pressure and abnormal cholesterol profiles
- Cardiomyopathy and heart rhythm disorders
- Increased risk of blood clots
Liver damage
- Especially with oral anabolic steroids
- Can permanently damage the liver
- Risk of liver tumors and cyst development
- Elevated liver enzymes and jaundice
Endocrine disorders
- Suppressed natural testosterone production
- Testicular atrophy and infertility
- Gynecomastia (enlarged breasts in men)
- Growth disorders in adolescents
Psychological side effects
Abuse of high doses of testosterone and other anabolic steroids can have serious psychological consequences:
Aggressive behavior and “roid rage”
- Increased irritability and aggression
- Violent behavior and social conflicts
- Impaired impulse control
Mood swings and psychiatric symptoms
- Depression and anxiety
- Manic episodes
- Psychosis in rare cases
- Increased risk of suicide
Dependence and withdrawal
- Psychological dependence on the effects
- Withdrawal symptoms upon cessation: depression, fatigue, loss of muscle mass
- Difficulty in quitting despite negative consequences
Long-term consequences
The long-term consequences of steroid abuse can be irreversible:
- Permanent damage to natural hormone production
- Increased risk of prostate cancer
- Accelerated aging and increased mortality
- Social and economic consequences
- Legal problems with illegal use
Testosterone in women
Although testosterone is often considered the male sex hormone, it also plays an important role in women. Understanding the function of testosterone in women is essential for optimal hormone balance and health.
Women's natural testosterone production
Women produce testosterone in smaller amounts than men, but the hormone is still essential for several physiological functions:
Production Sites
- Ovaries: Produce about 25% of women's testosterone
- Adrenal glands: Contribute about 25%
- Peripheral conversion: The rest is produced in tissues such as skin and fat through the conversion of other hormones
Normal levels in women
- Premenopausal women: 15-70 ng/dL
- Postmenopausal women: Lower levels due to decreased ovarian production
- Varies throughout the menstrual cycle with highest levels around ovulation
The role of testosterone in women's health
Libido and Sexual Function
- Testosterone affects women's sex drive and sexual response
- Low levels can lead to decreased libido and sexual problems
- Important for sexual arousal and orgasmic function
Muscle mass and bone strength
- Helps maintain muscle mass and strength
- Supports bone mineral density and prevents osteoporosis
- Affects body composition and metabolism
Energy and mental well-being
- Contributes to energy levels and vitality
- May affect mood and cognitive function
- Role in motivation and drive
Causes of low testosterone in women
Menopause
- Natural decline in ovarian production after menopause
- Can lead to significant symptoms
- Often overlooked in medical treatment
PCOS (Polycystic Ovary Syndrome)
- Paradoxically, PCOS can lead to both high and low testosterone
- Complex hormonal disorder
- Requires specialized treatment
Other causes
- Surgical removal of ovaries
- Adrenal insufficiency
- Pituitary disorders
- Medications such as oral contraceptives
Treatment options for women
Testosterone treatment for women is less well established than in men and requires specialized assessment:
Indications
- Documented low testosterone levels
- Symptoms of androgen deficiency
- Lack of response to other treatments
Treatment modalities
- Low-dose testosterone gel or cream
- Combination therapy with estrogen
- Monitoring for masculinizing side effects
Special considerations
- Risk of masculinizing effects in case of overdose
- Interaction with other hormone treatments
- Need for specialized hormone expertise
Future perspectives and research
The field of testosterone research is constantly evolving, with new discoveries about the hormone's role in health and disease. Future research directions will shape how we understand and treat testosterone deficiency.
Ongoing research
Aging and Hormone Therapy
- Large Clinical Trials Examine Benefits and Risks of Testosterone Therapy in Older Men
- Focus on Cardiovascular Safety and Long-Term Effects
- Personalized Medicine Based on Genetic Factors
New Biomarkers
- Research into Advanced Methods to Measure Biologically Active Testosterone
- Better Diagnostic Tools to Identify Men Who Will Benefit from Treatment
- Integrating Symptom Scores and Laboratory Findings
New treatments under development
Improved delivery methods
- Longer-acting injectable formulations
- Improved transdermal systems with reduced risk of transfer
- Oral testosterone preparations with better absorption
Selective androgen receptor modulators (SARMs)
- Designed to provide anabolic benefits without androgenic side effects
- Potential use in muscle wasting and osteoporosis
- Still in clinical development and not approved for clinical use
The controversies surrounding testosterone therapy
The evidence base
- Debate on when treatment is indicated
- Lack of long-term safety data
- Need for better patient selection criteria
Anti-aging versus medication
- The difference between treating disease and optimizing health
- Ethical considerations around hormone therapy in healthy older adults
- Commercialization of testosterone therapy
- Behovet for større studier
The future of testosterone therapy depends on large, long-term studies that can answer important questions:
-
Long-term safety in different patient groups
-
Optimal treatment strategies and dosing regimens
-
Identifying patients who will benefit most from treatment
-
Cost-effectiveness of different treatment approaches
Conclusion
Testosterone is much more than just the male sex hormone - it is a fundamental regulator of many vital bodily functions in both men and women. From its role in the development of secondary sex characteristics to its impact on muscle mass, bone strength, libido and mental well-being, testosterone affects almost every aspect of our physiology.
Through this comprehensive review, we have seen how testosterone levels naturally decline with age and how lifestyle factors such as obesity, sleep deprivation and chronic stress can accelerate this decline. The symptoms of low testosterone can be subtle but have a significant impact on quality of life and include everything from decreased muscle mass and increased fatigue to decreased libido and mood swings.
The diagnosis of testosterone deficiency requires careful medical evaluation combined with laboratory measurements, and treatment should always be individualized under medical supervision. While medical testosterone therapy can be life-transforming for men with true deficiency, it is important to be aware of potential side effects and contraindications.
For many men, natural approaches such as weight loss, regular exercise, optimized sleep, and a healthy diet can be effective ways to support testosterone production. Supplements such as Tongkat Ali, zinc, vitamin D, and magnesium can also be beneficial in cases of proven deficiency.
It is crucial to distinguish between legitimate medical treatment and anabolic steroid abuse, which can have serious and potentially life-threatening consequences. It is also important to recognize the role of testosterone in women and the need for specialized evaluation for hormonal imbalances.
If you are experiencing symptoms that could indicate low testosterone, the most important step is to seek professional medical advice. A qualified physician can help assess your symptoms, conduct appropriate tests, and develop an individualized treatment plan that takes into account your overall health and goals.
The future of testosterone research looks promising with new treatment methods being developed and a better understanding of who will benefit from treatment. By combining evidence-based medicine with a healthy lifestyle, we can optimize hormone balance and improve quality of life throughout all stages of life.